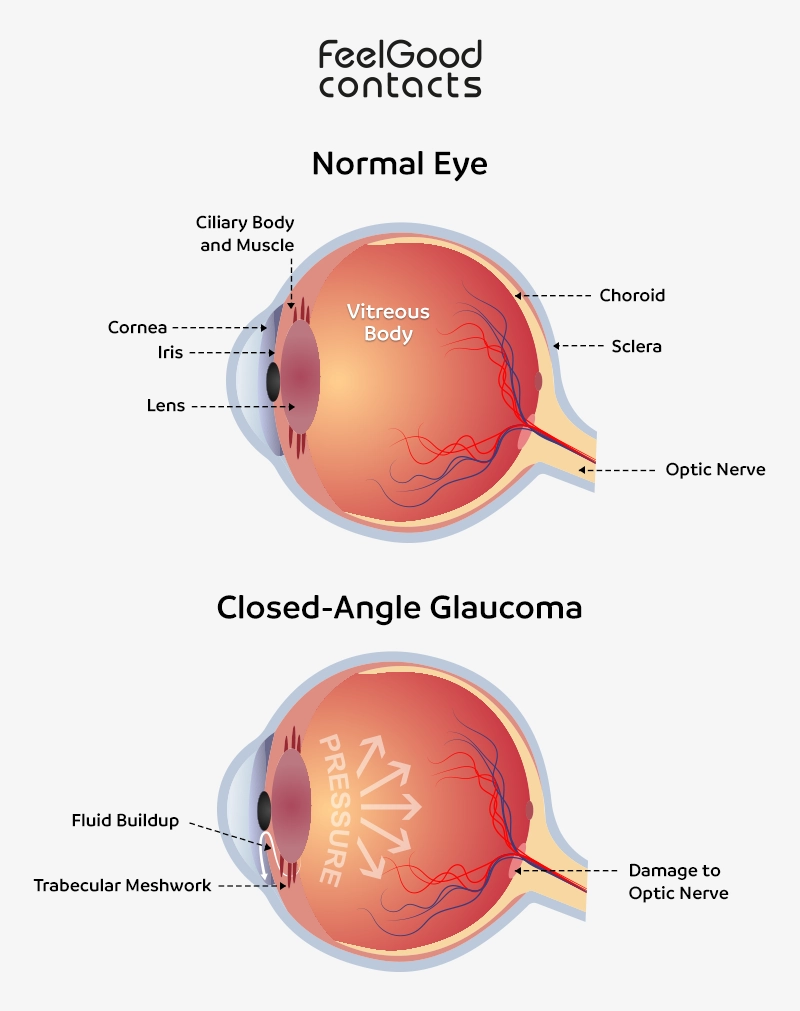
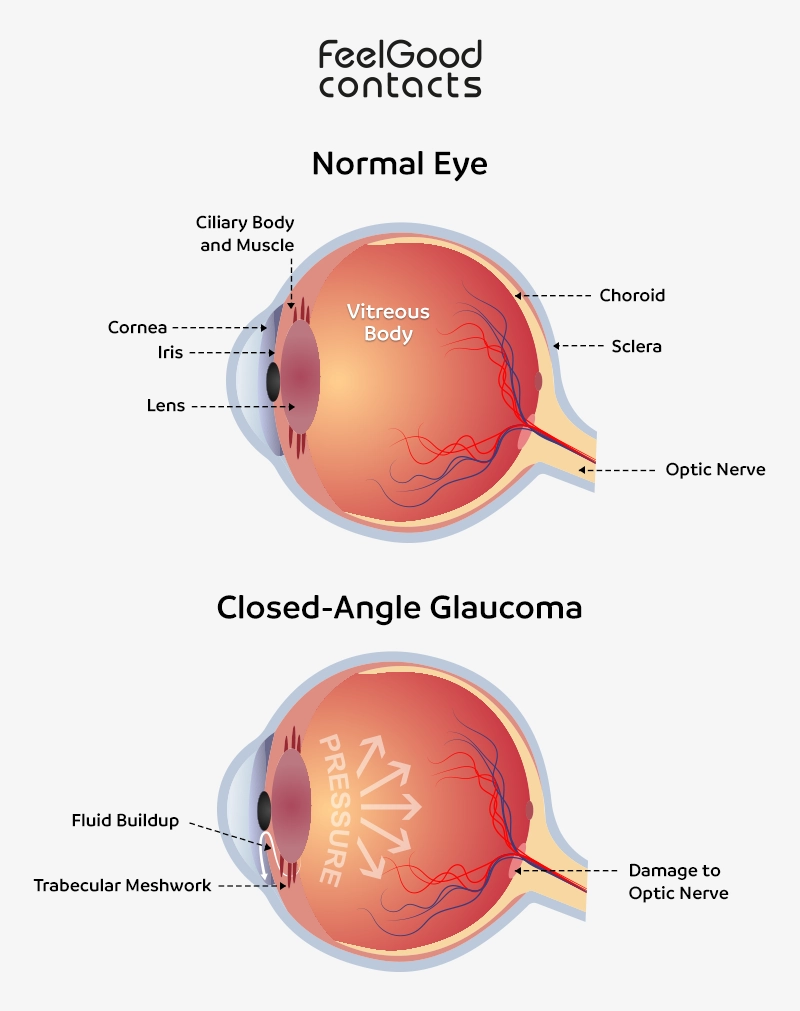
A key part of the mechanism in angle-closure glaucoma (sometimes referred to as narrow-angle glaucoma or closed-angle glaucoma) is the movement of the iris (the coloured part of the eye), which blocks the eye’s drainage pathways. In this condition, the fluid (aqueous humour) continually produced to maintain pressure cannot leave the eye, dramatically increasing intraocular pressure (IOP). If left untreated, the optic nerve degenerates quickly, leading to irreversible vision loss.
Angle-closure glaucoma may develop suddenly in an acute attack, referred to as acute angle closure glaucoma, causing a rapid rise in IOP, pain and vision loss. Attacks usually occur in the evening when the pupil is mid-dilated and the iris, being most bowed into the angle, further pushes the iris into the angle, blocks it and increases pressure through a positive feedback mechanism.
Angle-closure glaucoma causes
When the iris is anatomically very close to the drainage angle of the eye, it may block the drainage angle, preventing the fluid from flowing out of the eye. This anatomy can be due to:
- Smaller eyes have more cramped structures. Hypermetropic or ‘long-sighted’ eyes are at greater risk.
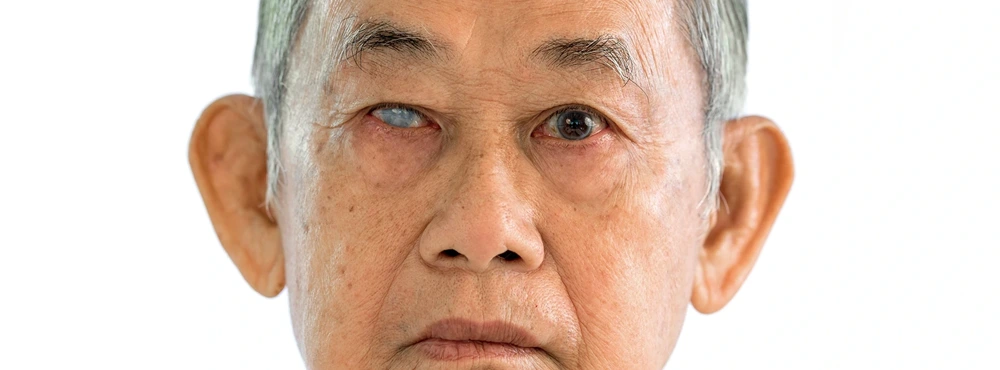
- The older a person is, the larger their lens. The lens within the eye is one of the few things that continues to grow throughout life, like hair or nails. However, eyes do not grow. Therefore, with an ageing population, more people are likely to have lenses that effectively outgrow their eyes.
- During embryonic development, the angle structures sometimes may not form completely, leading to shallow angles that are more prone to closure.
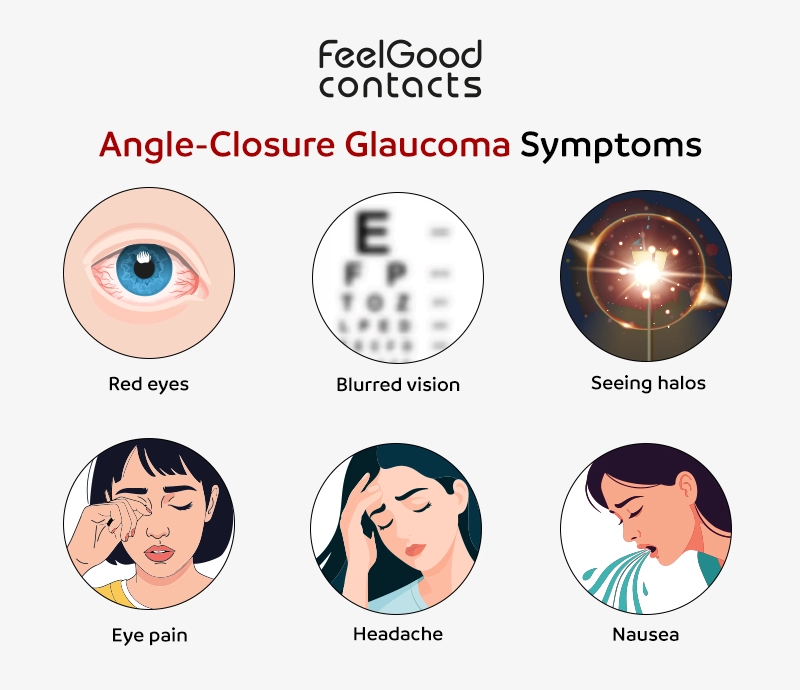
Angle-closure glaucoma symptoms
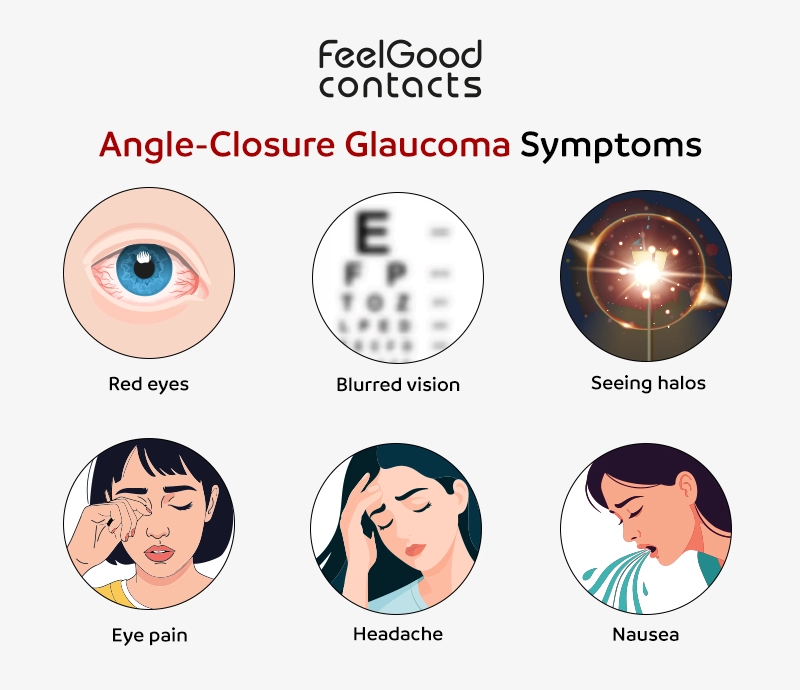
Angle-closure glaucoma can develop slowly without symptoms or suddenly with severe eye pain, haloes and vision loss (see below). Without symptoms, the person may remain unaware until optic nerve damage is severe. Early detection of angle-closure glaucoma signs is crucial to prevent permanent vision loss.
Possible symptoms of angle-closure glaucoma include:
- Eye discomfort
- Blurry or low vision
- Red eyes
- Seeing halos (rainbow-coloured rings around lights)
- Severe eye pain
- Bad headache or eyebrow pain
- Nausea or vomiting
- Permanent vision loss
Treatment for angle-closure glaucoma
The ultimate treatment for angle-closure glaucoma is cataract surgery, in which the natural lens that has grown too big for the eye is removed and replaced with a clear plastic lens that takes up less space. A piece of plastic is not going to grow; therefore, this remedies the problem for most people.
However, cataract surgery is not without risk, especially in eyes with a small axial length, where there is limited space to manoeuvre instruments, and the eye’s fluid dynamics are often challenging during surgery.
An alternative option to ‘buy time’ after the intraocular pressure has been brought down with medication is to perform Laser Peripheral Iridotomy (LPI). This is a procedure in which a tiny hole is created in the iris with a laser. This stops the sudden clogging of the drainage pathway. However, this will not stop the lens growing and may later cause problems with pressure.
Prevention of angle-closure glaucoma
Angle-closure glaucoma cannot be prevented. However, early detection and treatment can help manage eye pressure and possibly delay or prevent vision loss.
Alastair Lockwood, an Eye Health Advisor at Feel Good Contacts, suggests the following ways that can help identify angle-closure glaucoma early.
- Get regular eye exams: Regular eye exams can help you determine your risk for this condition, as they can detect an increase or risk of an increase in eye pressure even before the symptoms of angle-closure glaucoma appear. Your eye care provider can then recommend appropriate treatments to reduce the risk.
- Know your family’s eye health history: As this condition is hereditary, those with a family history of glaucoma are recommended to have eye tests more frequently.
- Use eye drops regularly: Use your prescribed eye drops regularly if you have been diagnosed with glaucoma, even if you don’t have any symptoms, as it can significantly reduce the risk of progression or vision loss.
Frequently asked questions
Can angle-closure glaucoma cause blindness?
If left untreated, angle-closure glaucoma can lead to blindness or permanent vision loss within days. Timely treatment can help patients avoid serious complications.
Can I go blind even after my angle-closure glaucoma is treated?
The risk of becoming legally blind is quite low if you follow your treatment plan and go for regular follow-up appointments as directed by your optician. With proper eye care, vision loss can be avoided.
Can angle-closure glaucoma return after laser surgery?
Laser surgery buys time and may be enough to hold off problems with glaucoma for many years. However, the natural lens within the eye can still cause problems, as it grows later in life. Regular follow-up visits ensure that intraocular pressure remains normal and the drainage angle in the eye stays clear.
Can I drive after my angle-closure glaucoma is treated?
Most individuals who have been successfully treated for angle-closure glaucoma can drive safely. However, those who have lost their peripheral vision might be required to take a driving test field test, which is evaluated by DVLA (Driver and Vehicle Licensing Agency).
Disclaimer: The advice in this article is for informational purposes only and does not replace medical care or an in-person check-up. Please check with an eye care professional before purchasing any products or remedies. For information on our article review process, please refer to our Editorial Policy.

 Offers
Offers Account
Account
 Favorite
Favorite
 Basket
Basket

 OFFERS
OFFERS